It can be hard to understand and respond to a RAD behavior. Reactive Attachment Disorder is complex.
There are times that you may question if you're seeing what's really happening.
In these moments it's always important to give the child the benefit of the doubt.
It can be so easy to think differently when you're the target.
Assume that your child with Reactive Attachment Disorder has the best of intentions.
There's always a chance that something else is going on.
When there are unsafe situations occurring, I follow 4 steps to understanding RAD behaviors.
There are so many reasons a child may act the way she does.
And quite frankly all of the things mentioned in this post can be going on at once!
This is why I always follow these steps when things escalate.
4 Steps to Understanding RAD Behaviors
Warning: This
post contains content related to Reactive Attachment Disorder that may be
triggering to some.
Important: Children with RAD are
victims of abuse and/or neglect. Behaviors associated with Reactive Attachment
Disorder are due to how the brain forms while the innocent child is surviving
trauma. It is our goal to support healthy and loving families where children
with RAD can heal, if possible.
1. Seek Medical Attention
Our bodies are complex. We can't always see what's going on beneath the surface.
Seeking medical attention from a PCP or psychiatrist to eliminate the possibility of health issues is so important when seeing an increase in behaviors that could be related to RAD.
Sunshine's last mental health crisis was a result of her thyroid acting up. She needed an increase in medication.
A thyroid that's not working properly can cause extreme irritability.
Sunshine also needed some med adjustments.
With every new and reoccurring behavior, give the child with Reactive Attachment Disorder the benefit of the doubt.
I can't tell you how many times Sunshine has felt sick with an ear infection, and I didn't know it, and that's why she wasn't okay.
When it comes to personal hygiene issues, check for infections first before giving consequences.
Don't always assume that behaviors are related to Reactive Attachment Disorder.
Check in with a psychologist, developmental pediatrician, or other professional to ensure nothing else is going on regarding the child's mental health.
A child changes as she develops and grows.
Meds may need to be altered with a growth spurt.
New diagnoses may come.
Some diagnoses may be removed.
There may be a medical reason for the increase in behaviors.
Be sure to document behaviors in preparation for an appointment, so professionals or specialists have all of the information they need to help you.
If there are no medical explanations for an increase in RAD behaviors, move on to step two.
Remember no child has control over medical challenges going on with their body, and just like adults, these struggles affect functioning.
2. Meet Sensory Needs
A child with Reactive Attachment Disorder is human, just like everyone else.
She has sensory needs.
When sensory needs are not met, behaviors escalate.
Identify how your child with Reactive Attachment Disorder responds to the senses and how your child prefers to regulate those senses.
Is she hypersensitive or hyposensitive to different senses?
It is completely normal for a child to be hypersensitive to one sense and hyposensitive to another.
If you are unfamiliar with the 8 senses, I have listed them below.
Take the time to understand them and how they relate to your child.
List of the 8 Senses
- Tactile (touch)
- Auditory (sound)
- Gustatory (taste)
- Visual (sight)
- Olfactory (smell)
- Proprioceptive (have to do with deep pressure and feelings of internal muscles)
- Vestibular (having to do with balance and the inner ear)
- Interoception (having to do with how the body responds to pain, bodily functions, etc.)
Be aware that trauma influences the senses.
Abuse, neglect, and medical procedures have a huge impact on how the body responds to the world around it.
Assume that sensory struggles are at play, accept that sensory struggles are real, and work to meet needs, before thinking that behaviors are only related to Reactive Attachment Disorder.
Help the child feel safe in the environment by meeting sensory needs.
Also pay attention to your own sensory needs. Be sure to meet those needs in the process, so you are better able to co-regulate.
Meeting sensory needs is the first step to helping a child with RAD feel safe.
No matter what type of trauma a child with Reactive Attachment Disorder experienced in utero and during the first 18 months of life, sensory needs weren't met.
There is a chance that when those needs are met, that the child with RAD will feel safer and behaviors may diminish.
3. Provide Help with Emotional Dysregulation
Once you have checked into medical issues and met sensory needs, the behavior that is perceived to be related to RAD, still may not be about Reactive Attachment Disorder at all.
It could be about emotional dysregulation.
All of us have emotions.
When emotions become larger than a person can cope with, a person becomes dysregulated.
A child with Reactive Attachment Disorder struggles with regulating emotions even when life appears calm.
If life has included hiccups, triggers, or changes recently, it could be that your child is emotionally dysregulated, unable to handle the emotions she is feeling.
She may be trying to express emotions in the best way she knows how in the moment.
All behavior is communication.
When feeling emotionally dysregulated, a child's ability to communicate effectively and appropriately lessens. It may be absolutely impossible depending on the triggers.
Provide supports when needed.
Support may come in the form of co-regulation.
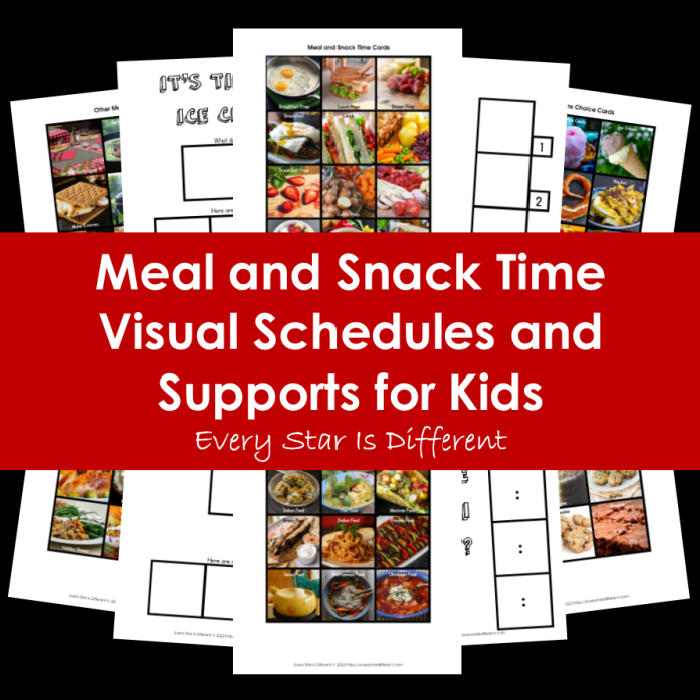
Visual schedules and social stories may help.
Sometimes tangible objects like sound blocking headphones, chewies, or other resources may be necessary.
Necessary supports may be related to the senses.
Breathing exercises and visuals that express emotions may be helpful.
4. It's a RAD Behavior
Once I have eliminated the possibility of all of the options listed above for a behavior, I will consider that the behavior is related to RAD, IF my child has a diagnosis of Reactive Attachment Disorder that has been confirmed by two or more professionals and/or specialists.
Both of our girls have been seen by multiple professionals and specialists that have confirmed the diagnosis.
We continue to see these professionals regularly to ensure that we remain informed on any changes.
If you do not have a confirmed diagnosis of RAD from at least two professionals or specialists, go back to step one of this list.
It is incredibly dangerous to assume that behaviors are related to Reactive Attachment Disorder without that confirmed diagnosis.
What Is A RAD Behavior?
A behavior triggered by Reactive Attachment Disorder is a behavior that has occurred because a child feels unsafe with the amount of love, affection, and/or attention she is receiving.
A child with RAD struggles with attachment. She is unable to attach to caregivers, which means she does not trust them to care for her.
A child with Reactive Attachment Disorder will do anything she can to push people away when she feels unsafe while others are trying to form secure attachments with her.
Reactive Attachment Disorder is on a spectrum. Some children with RAD do not display behaviors to the degree of others.
Treatment for Reactive Attachment Disorder looks so differently than other emotional and developmental diagnoses.
I will consider a behavior RAD related ONLY after I've done all I can to help my child with the three steps above.
This means listening to the advice of well intentioned professionals whom I trust.
Once I know a behavior is related to Reactive Attachment Disorder, I will treat it as such.
Treatment looks different with every child with RAD.
I have two daughters with Reactive Attachment Disorder.
Their trauma experiences are opposite of each other.
Their responses to the world around them are opposite of each other.
What they need from me differs in every situation.
Responses to RAD behaviors will look different depending on the child.
There are definite responses that are not appropriate though.
I understand that it can be extremely challenging living with a child with Reactive Attachment Disorder, because behaviors can be so extreme.
It's so easy to say, that a particular incident is RAD related, without pause, because so many behaviors are.
When we do pause to take perspective, working through the steps above, before giving natural and logical consequences for actions, we are helping our child and ourselves.
Hang in there.
Behaviors related to Reactive Attachment Disorder can be scary and dangerous.
Focus on safety!
Remember that the best treatment for RAD comes from the family unit.
I do believe over time that a child can heal, if she chooses, because I've seen it happen in my oldest daughter.
Never give up hope!
If you enjoyed this post, you may also like the resources below.
















.jpg)
No comments:
Post a Comment